Case 2
Clinical Stem:
You are a fourth-year medical student on your emergency medicine rotation in Lethbridge. A 24-year-old male presents to the emergency department with sudden-onset right-sided chest pain and shortness of breath that began approximately one hour ago while he was smoking with some friends. He describes the pain as sharp and pleuritic in nature. It is localized to the right side of his chest. It is worse with deep breaths. He denies any trauma, fever, cough, or recent illness. He is tall and thin, with no significant past medical history and no known lung disease. He is otherwise healthy.
Vital Signs:
-
Temperature: 36.8°C
-
Heart Rate: 110 bpm
-
Respiratory Rate: 24 breaths/min
-
Blood Pressure: 124/78 mmHg
-
SpO₂: 96% on room air
On Physical Exam:
-
The patient appears mildly distressed and is taking shallow breaths.
-
Decreased chest expansion on the right
-
Hyperresonance to percussion on the right
-
Diminished breath sounds over the right lung field
-
No tracheal deviation or subcutaneous emphysema is noted
Your preceptor asks you to order an upright PA and lateral chest X-ray to investigate further.
Question:
Review the provided chest X-ray. What are the radiographic findings, and what is your most likely diagnosis?
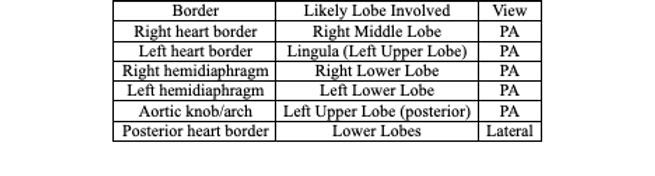
PA View
Dixon, A. (n.d.). Radiopaedia case rID: 48365. Radiopaedia.org. https://radiopaedia.org/cases/48365?lang=us
Chest X-Ray Interpretation Using RIPE + ABCDE
Step 1: R.I.P.E. – Technical Adequacy
-
Rotation
-
Clavicles are equidistant from the spinous processes.
-
Not rotated → accurate anatomical relationships.
-
-
Inspiration
-
9-10 posterior ribs visible above the diaphragm.
-
Good inspiratory effort.
-
-
Projection
-
Posterior-Anterior (PA) view.
-
Heart size is reliable here.
-
-
Exposure
-
Vertebral bodies visible behind the heart shadow.
-
Adequately penetrated.
-
Step 2: A – Airway & Mediastinum
-
Trachea is midline, no deviation.
-
Carina visible, no airway obstruction.
-
No mediastinal widening or silhouette signs.
-
No signs of tracheal shift to suggest tension physiology.
Step 3: B – Breathing (Lungs & Pleura)
-
Clear pleural line visible in the upper right hemithorax with absence of peripheral vascular markings beyond it → consistent with right-sided pneumothorax.
-
Remaining right lung appears partially collapsed.
-
No consolidation, nodules, or pleural effusion.
-
Lung markings preserved on the left side.
-
Pleural spaces otherwise unremarkable.
Step 4: C – Circulation (Heart & Vessels)
-
Heart size is normal (cardiothoracic ratio <50% on PA view).
-
Right and left heart borders are well defined.
-
No silhouette sign → no adjacent parenchymal pathology.
-
Aortic knob and pulmonary vasculature are unremarkable
Step 5: D – Diaphragm
-
Right hemidiaphragm is higher than the left (normal anatomical variant).
-
No free air under either hemidiaphragm.
-
Costophrenic angles are sharp and clear → no evidence of pleural effusion.
-
Gastric bubble present under the left hemidiaphragm.
Step 6: E – Everything Else
-
Bones: No rib or clavicle fractures. Spine is intact.
-
Soft tissues: No subcutaneous emphysema or masses.
-
Lines/Devices: No lines, tubes, or devices seen in this image.
Summary
The chest X-ray reveals a moderate-sized right-sided pneumothorax, demonstrated by a visible visceral pleural edge and the absence of vascular markings in the peripheral right lung field beyond the pleural edge. There is no evidence of mediastinal shift, making tension physiology unlikely. No consolidation, effusion, or other acute pathology is identified.